Alzheimer’s research is expensive and doesn’t always produce a result. Alzheimer’s is complicated, and because of that, many companies are pulling back on research. Doing this is detrimental to everyone because it’s such a prevalent disease. Luckily, there are a lot of small companies taking up the mantle, and even trying a new angle by focusing on the immune system.

Small Companies Keeping Alzheimer’s Research Alive
Back in the 90s, a health-care startup called Partner Therapeutics made a leukemia drug called Luekine. Doctors barely prescribed it, and it faded away into obscurity until a group of researchers in Colorado brought it back. The Rocky Mountain Alzheimer’s Disease Center wanted to see if it can regulate the immune system as a way to battle Alzheimer’s.
Forty participants with Alzheimer’s will be part of the trail. In mice with this disease, the same protein in Luekine cleared amyloid debris from the brain while reversing memory loss. Though, the difference between humans and mice is vast, so we have to wait to know if it will do any good.
Many researchers and companies are looking at different ways to tackle the problem of Alzheimer’s since the usual research has come up with nothing.
Larger pharmaceutical companies have been backing out due to Alzheimer’s research failure. Biogen stopped a clinical trial in March after their latest experimental amyloid plaque drug fell flat. Stopping the test caused their stock to fall twenty-nine percent. Johnson & Johnson, Merck, Eli Lilly, and AstraZeneca have also had failures.
Last year there were more than 70 Alzheimer’s trials in different stages, plus 22 amyloid-targeting drugs were being tested. Compare that to the 1,100 drugs in development for cancer, 445 for other brain diseases, and 200 for heart disease and stroke.
Not all is lost, though. Drugs going after a different protein in the brain called tau protein tangles, anti-inflammation medications, immune modulators, gene therapy, insulin, and cannabis compounds are being looked into.
Immunity and Alzheimer’s
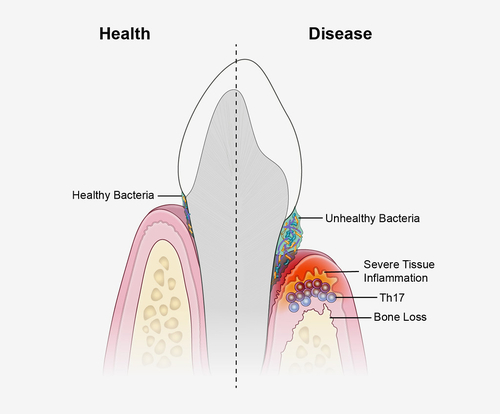
The immune system’s connection to Alzheimer’s has been an area of interest for a long time. Now, thanks to advances in human genome mapping, it’s possible to target the roles of specific genes. Three companies in California: Denali Therapeutics, Alector, and INmuneBio, are following this avenue. Too much inflammation, which is the immune system’s reaction to sickness, can cause damage to neurons and mess with the brain.
People at Alector think that researchers have spent too much time on getting rid of amyloid plaque, even though there is a lot of evidence saying it wasn’t working. They want to focus on drugs that help microglia do their job.
Denali is also looking into immunotherapy. They have created experimental molecules that can pass through a membrane called the blood-brain barrier. Doing this will let them affect the brain.
A Canadian company, IntelGenx, is doing a trial of an anti-inflammatory asthma drug called Montelukast. They changed its formula so that it can be taken as a dissolvable strip, making it easier for seniors and have the company stand out at the same time.
There are even more studies happening all over the world that are trying to tackle this problem from all different angles. So, while familiar names are backing away from this challenge, newer and younger names are stepping up.
Read more here.